Keratoconus (KC) is a condition where the cornea gradually becomes thinner and more irregular, which can blur and distort vision. This guide explains early signs, the key diagnostic tests, and today’s treatment options—without hype and without guesswork.
Last updated: 30/12/2025
Keratoconus (KC) is a condition where the cornea gradually becomes thinner and more irregular, which can blur and distort vision.
If you’ve noticed frequent prescription changes, halos at night, or distorted streetlights, the right scans can clarify what’s happening and whether the cornea is stable.
This guide explains early signs, the key diagnostic tests, and today’s treatment options—without hype and without guesswork.
Ready for clarity based on your corneal scans? Book an eye consultation at a Magrabi Health hospital in the UAE. to review your results and discuss next steps.
Keratoconus is when the normally dome-shaped cornea thins and bulges forward into a more cone-like shape. Because the cornea helps focus light, changes in its shape can cause blurred, distorted, or “shadowed” vision—especially as irregular astigmatism increases.
The exact cause is not always clear. Many people have a mix of genetic tendency plus environmental triggers (especially chronic eye rubbing and allergy-related irritation).
Even when keratoconus is mild, day-to-day conditions can amplify how your vision feels. In the UAE, a few common factors may make blur, glare, or discomfort more noticeable.
Air conditioning can contribute to tear-film instability, which can worsen fluctuating blur and glare.
Dusty days and seasonal allergies can increase itching, leading to more eye rubbing.
Long screen hours reduce blinking, which can worsen dryness-related visual fluctuation.
Night driving can highlight glare, halos, and “streaking,” especially with irregular corneal optics.
Early keratoconus is often missed because it can look like “just astigmatism.” These signs are worth checking—especially if they’re new or getting worse.
Frequent prescription changes, especially increasing astigmatism.
Ghosting/double images in one eye (monocular “shadowing”).
Distorted lights, streaks, halos, or glare—often worse at night.
Blur that doesn’t fully sharpen with glasses.
Increasing reliance on squinting to see road signs or screens.
Unequal vision between eyes that seems to widen over time.
Contact lens discomfort or reduced lens tolerance compared with before.
Risk is not a diagnosis—but it helps decide how early to scan and how closely to follow you.
Family history of keratoconus
Long-term eye rubbing (often linked to allergies/itching).
Atopy/allergic conditions (asthma, eczema, allergic rhinitis).
Certain general medical conditions your doctor may ask about (case-by-case).
A proper diagnosis is based on clinical examination plus corneal imaging. This is also how doctors detect very early disease and monitor progression over time.
Your doctor checks your prescription (refraction) and examines the cornea under a slit lamp for signs of thinning, irregularity, or scarring.
Topography maps the corneal surface shape; tomography evaluates shape in more depth (including the back surface) and can flag earlier changes. These scans are central to confirming keratoconus and assessing risk.
Thickness patterns matter—not only the “thin number.” Pachymetry and shape indices help assess severity and whether certain treatments are safe.
Treatment choices often depend on whether keratoconus is progressing. Repeat measurements (with consistent technique and timing) help determine if the cornea is stable or changing.
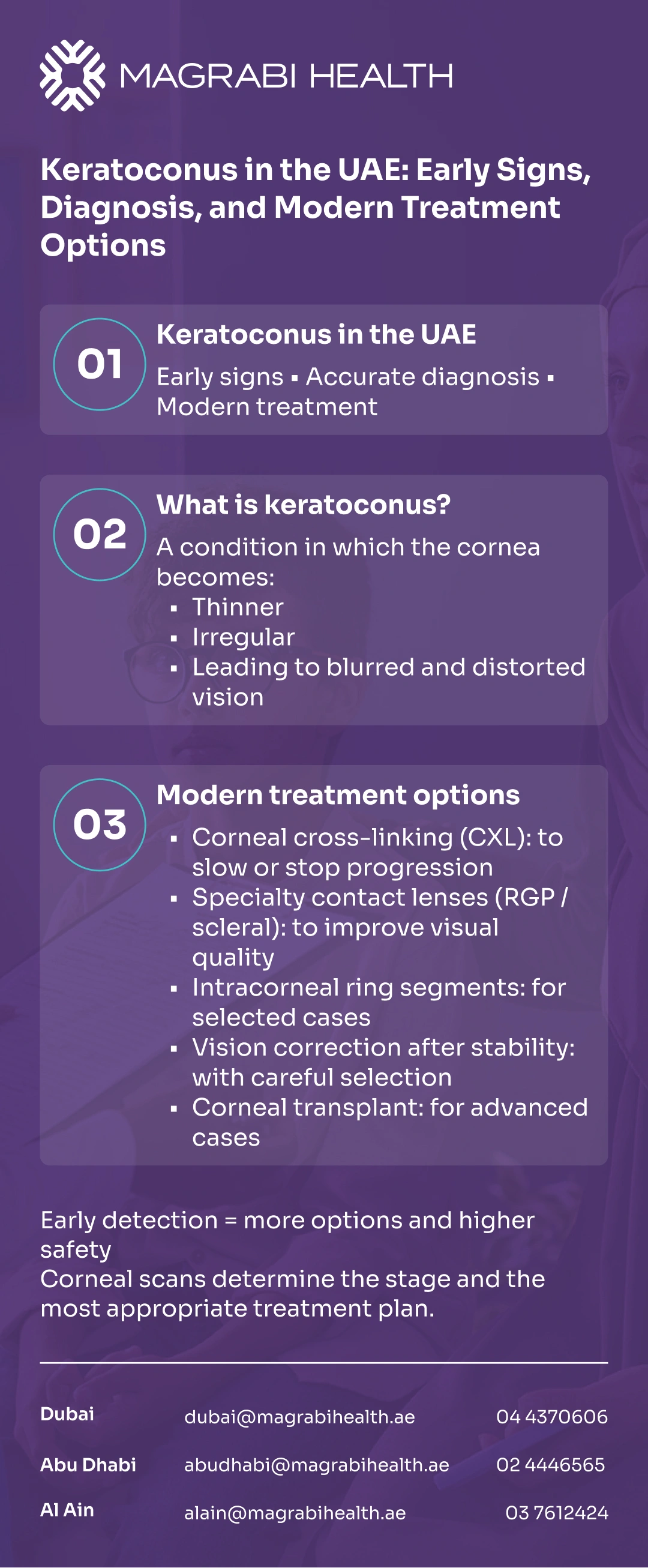
Keratoconus can progress slowly, and it may stabilize at different stages—mild, moderate, or advanced. The goal isn’t usually to “cure” the cornea, but to preserve vision, keep the cornea stable, and improve visual quality with the safest option for your stage.
A key mindset shift helps: treating progression (stability) is different from correcting vision (glasses/contacts or selective procedures). Many people still need glasses or contact lenses even after stability-focused treatment.
Treatment is personalized to your scans, symptoms, and stability—especially if you’re a student, heavy screen user, or frequent night driver in the UAE.
You can also visit the related service page on the Magrabi Health website to learn what a keratoconus assessment and treatment pathway may include.
Corneal Cross-Linking (CXL) is designed to slow or stop keratoconus from getting worse by strengthening corneal collagen. It’s commonly recommended when scans show progression and the cornea meets safety criteria.
CXL doesn’t usually eliminate the need for glasses or lenses, but it can protect long-term stability.
When glasses aren’t enough, specialty lenses can improve clarity by creating a smoother optical surface. Scleral lenses, in particular, vault over the cornea and can be helpful for irregular corneas like keratoconus.
Intracorneal ring segments (ICRS) are small implants placed within the cornea to help reshape it. They may improve lens tolerance and visual function in selected patients—your corneal thickness and scarring pattern matter.
After the cornea is stable, some carefully selected patients may be considered for options such as topography-guided surface laser in combination with stability treatment, or an implantable contact lens (ICL). These are not “one-size-fits-all” and require strict safety checks.
If keratoconus becomes advanced—especially with significant scarring or lens intolerance—corneal transplant procedures may be considered.
Newer cross-linking approaches that avoid removing the corneal epithelium are evolving. Availability and indications can differ by country.
For an overview of halo and glare assessment steps, you can visit the Refractive and Cornea Care services page on the official Magrabi Health Hospitals website.
Small adjustments can meaningfully improve day-to-day function—especially for students, office workers, and frequent night drivers in the UAE.
Dryness can make vision fluctuate, so focus on blinking, breaks, and optimizing your work setup. If you use lubricating drops, choose options recommended by your clinician for your eyes and contact lens type.
If halos and glare suddenly worsen, or you feel less confident at night, consider pausing night driving until your vision is assessed. Updating optics (prescription, lens fit) and addressing dryness can help, but scans are key when symptoms are changing.
Specialty keratoconus lenses need careful hygiene and planned follow-up to protect the cornea and keep vision reliable. If a lens becomes painful or your eye becomes red, don’t “push through” it—get checked.
Daily choices can support comfort and reduce triggers that may worsen symptoms. The biggest practical win is to reduce eye rubbing by addressing itch and irritation safely.
If you wear contacts, follow your fitting and follow-up plan closely—especially if your prescription keeps changing or your lens comfort drops.
Seek urgent eye care if you have sudden significant vision loss, severe pain, new marked light sensitivity, a rapidly increasing red eye, or a sudden cloudy/whitish haze—these can signal complications that need prompt assessment.
Keratoconus in the UAE is manageable when it’s detected early and monitored properly. If you recognize the early signs—especially frequent astigmatism changes or night glare—corneal scans can clarify whether the cornea is stable and which modern options fit your stage and lifestyle.
Concerned about progression or night-driving glare? Book an eye consultation at one of Magrabi Health’s hospital branches in the UAE—Dubai, Abu Dhabi, or Al Ain to review your scans and discuss a practical plan.
This article is for general education only and does not replace a medical diagnosis or personalized treatment plan. If you have new or worsening symptoms, please consult a qualified eye care professional.
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.
The guidance below reflects established patient information from major eye and health organizations.
American Academy of Ophthalmology (AAO) — What Is Keratoconus?
Moorfields Eye Hospital (NHS) — Keratoconus: Diagnosis and treatment.
Moorfields Eye Hospital (NHS) — Corneal cross-linking.
American Academy of Ophthalmology — Technology assessment: cross-linking effectiveness.

What Makes an Eye Hospital in Dubai Truly Stand Out?