When keratoconus is progressing, the focus often shifts from “perfect vision today” to protecting vision options for the future. CXL is designed to stabilise a weakening cornea so the condition is less likely to worsen. This guide explains how it works, who it helps, and what to expect in the UAE.
Last updated: 05/01/2026
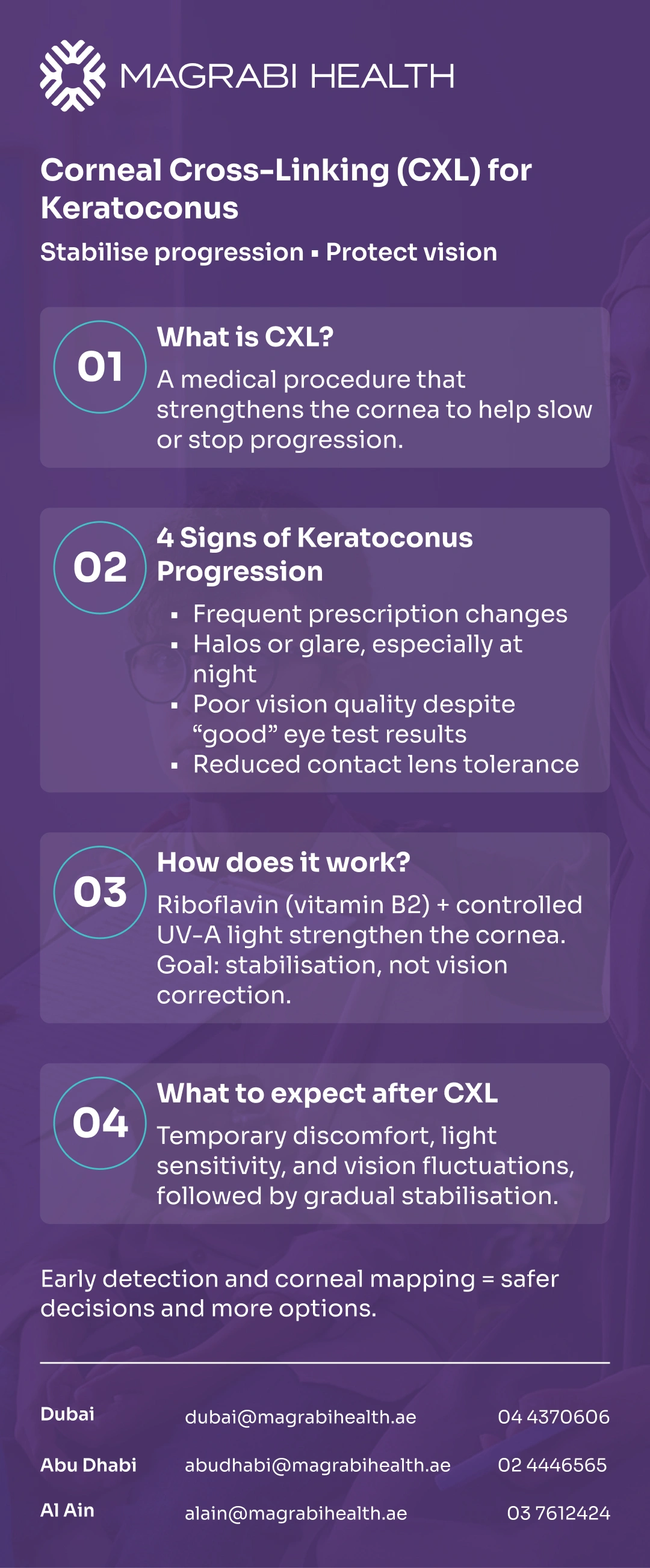
Corneal cross-linking (CXL) is a disease-stabilising treatment for keratoconus that strengthens the cornea and helps reduce the risk of further bulging and thinning.
Keratoconus can feel unpredictable—your prescription may change, night driving may become stressful, and contact lens comfort can decline, especially with long screen hours and air-conditioned environments common in the UAE.
When keratoconus is progressing, the focus often shifts from “perfect vision today” to protecting vision options for the future. CXL is designed to stabilise a weakening cornea so the condition is less likely to worsen.
This guide explains how it works, who it helps, and what to expect in the UAE.
Concerned about keratoconus progression? Book an eye consultation at a Magrabi Health hospital in the UAE to review your corneal scans and discuss whether CXL may be appropriate.
Corneal cross-linking (CXL) is a procedure that strengthens the cornea using riboflavin (vitamin B2) drops activated by ultraviolet-A (UV-A) light. The purpose is to increase corneal rigidity and reduce the likelihood that keratoconus (or corneal ectasia) continues to worsen.
CXL is best understood as a stabilisation treatment. It is not primarily a “vision correction” procedure, and it does not promise to make the cornea return to a perfectly normal shape.
Keratoconus is a condition where the cornea becomes thinner and changes shape over time, leading to irregular astigmatism and reduced visual quality.
This progression is often more active in younger patients, and it may continue even when symptoms feel “stable” for a while.
In real life, progression may show up as:
Frequent prescription updates
Increasing ghosting, halos, or glare
Worse quality of vision despite “good numbers” on the eye chart
Reduced contact lens tolerance
CXL works at the tissue level to help the cornea resist deformation.
Under controlled conditions, riboflavin and UV-A light trigger chemical bonds (cross-links) between collagen structures within the cornea, increasing biomechanical stability.
CXL is designed to slow or stop worsening. It may reduce the need for more invasive surgery in some patients, but it does not guarantee you won’t need glasses, contact lenses, or additional treatments later.
Doctors recommend CXL most often when keratoconus is progressive or when the risk of progression is significant.
Common reasons specialists consider CXL include:
Documented progression on corneal mapping (topography/tomography).
Progressive keratoconus in adolescents/young adults.
Post-refractive surgery ectasia (in selected cases).
A keratoconus consultation typically includes refraction, slit-lamp exam, corneal topography/tomography, and corneal thickness measurement to confirm both diagnosis and safety.
Too Thin for LASIK? Safe Vision Correction Options for Thin Corneas and Keratoconus.
Timing is one of the most important parts of CXL decision-making. CXL is often most helpful before keratoconus reaches more advanced distortion—because the aim is to protect the cornea from continuing to change.
In many practices, the decision is driven by measurable change (your scans over time), not only by how you “feel” day to day.
You can also visit the relevant service page on the Magrabi Health website to learn what a keratoconus assessment typically includes.
CXL is typically a day procedure. The eye is numbed with drops, and the treatment is done under strict protocol and monitoring.
The established standard approach has traditionally involved removing the corneal epithelium (“epi-off”) to improve riboflavin penetration before UV-A exposure.
Newer “epi-on” approaches are being developed and evaluated, and regulatory approvals may vary by country and patient profile.
Before proceeding, your specialist checks corneal thickness, corneal shape, and overall eye health to reduce risk and confirm suitability.
Recovery varies, and it helps to plan around work, driving, and screen time.
In the early days, many patients experience discomfort, light sensitivity, and blurred vision (especially with epi-off). Over the following weeks, vision may fluctuate before stabilising.
Practical UAE-relevant tips your doctor may discuss:
Managing dry eye in air-conditioned environments.
Using preservative-free lubricants if advised.
Avoiding dusty outdoor environments during early healing.
Planning time off if your job requires heavy screen use or night driving.
For an overview of keratoconus assessment and CXL eligibility, visit the Refractive and Cornea Care service page on the Magrabi Health website.
Some people notice modest improvement in vision quality as the cornea stabilises, but outcomes differ. It’s common to still need glasses or contact lenses after healing.
Many patients pursue a step-wise plan:
Stabilise progression with CXL.
Optimise vision with updated glasses or speciality lenses.
Consider other options later (only if scans and stability allow).
All procedures have risks, and the exact risk profile depends on technique, corneal thickness, and individual healing.
Possible issues can include delayed surface healing, infection risk (particularly early after epi-off), temporary corneal haze, and visual fluctuations. Serious complications are uncommon with proper protocols and follow-up.
Your ophthalmologist should discuss realistic goals: CXL aims to stabilise, not to promise a specific vision outcome.
After CXL (or at any time with keratoconus), seek urgent review if you have:
Severe or worsening pain
Rapidly decreasing vision
Increasing redness or discharge
Marked light sensitivity that feels worse, not better
New “white spot” on the cornea or concern for infection
These symptoms don’t always mean a serious problem, but they warrant prompt assessment.
Corneal cross-linking (CXL) is a disease-stabilising treatment designed to slow or stop keratoconus progression by strengthening the cornea.
The most important decision factors are documented progression, corneal safety measurements, and realistic expectations—especially for patients in the UAE balancing screens, air conditioning, and night driving needs.
Do you feel your keratoconus may be progressing?
Book a consultation at one of Magrabi Health Hospitals to review your corneal maps and discuss stabilisation options such as CXL.
This article is for educational purposes only and does not replace a personalised medical evaluation. Diagnosis and treatment decisions should be made with a qualified ophthalmologist based on your examination and corneal scans.
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.
American Academy of Ophthalmology (AAO) — Corneal Cross-Linking (patient guidance). American Academy of Ophthalmology
Moorfields Eye Hospital (NHS) — Corneal cross-linking for keratoconus. Moorfields Eye Hospital
Imperial College Healthcare NHS Trust — Corneal cross-linking patient leaflet (PDF). Imperial College Healthcare
NICE — Photochemical corneal collagen cross-linkage evidence (riboflavin + UV-A).NICE

Step-by-Step Guide to Refractive Surgery Evaluation at Magrabi

What Are Refractive Errors? Causes, Types and Symptoms Explained